Did you catch my double entendre in the title? Trying to be a clever writer and failing with pride ha ha ha!
Anyway, one can well imagine that I have become very comfortable in ICU with Michael officially reaching the 10 day mark of his stay. I'm at hospital for about 5 hours every day. I pop in to see Michael for 10 to 30 minutes at a time, depending on what's happening in the ward, and the rest of my time is spent either expressing or working in the waiting area.
I have gotten to know some of the nurses who tell me about their kids, their pets, their favourite foods and favourite funny videos on Facebook. They also tell me amazing stories about memorable patients; babies and children who survive against all odds or interesting situations they have experience in surgical ICU. The team is quite a wonderful group and they're all very relaxed and friendly. Michael has been a case study for three nurses who are completing their course on paediatric cardiothoracic work and I happily gave consent because there's no harm in helping to further the education of enthusiastic healthcare professionals.
I'm also getting to know some of the parents of other patients. There's Casey who I have written about before. We message and email each other to check in on our kids' progress. I met Christina just yesterday after her son had surgery. He's 5 and the nurses say it's not often they get a preschooler patient. He's the big kid among all the babies and the newest "tenant" in the ward. There's only one girl in the ward and I've told the nurses I haven't had the courage to speak to her parents yet. They always look stressed but the nurses have said maybe a friendly chat with another parent may help them and make them feel a bit more assured, especially because their little girl is improving rapidly after quite a scare last week. Finally, there's the ward's smallest but currently most senior patient because he's been there the longest. He's only a month old and he's been there for almost all of that time. I finally spoke to his mom today and now I'm helping her to find new accommodation in Cape Town as she's here from East London.
I know I'm not the first parent whose child has been there for an extended stay but it makes things a lot easier being comfortable with the people who care for my child in this time. My way of making the best of a situation has always been to integrate myself with the people and thankfully I've encountered really nice people so far. Also, we are going to be back for Michael's second surgery next year and at least we'll be going back into a situation we now know and trust.
While I am trying to not be a nuisance and also choosing to have some days where I only visit once, ICU has become a bit of a second home filled with interesting aunties, quiet children I can only gaze upon from the safe zone of Michael's bassinet, the melodic beeps and flashing colours of the monitors and the oh so unforgettable scent of antibacterial gel.
Just a little drama
Michael is definitely giving us one helluva adventure in hospital.
The week was fairly tricky and he started to look like me might show improvement over the weekend. Well, we were wrong. The nurses tried over a few days to get Michael off the respirator because he wasn't requiring any additional air, just some pressure assistance. If he was breathing on his own, it was logical to take him off the machines.
The attempt on Saturday morning didn't go well. He reacted badly and ended up being put back on the ventilator to give him a rest and he needed a visit from the cardiologist. While the suspicion was that there was fluid around his heart, it turned out that his heart was fine and there was in fact fluid around his lungs. He got some medication to encourage the fluid to be absorbed and flushed out and he was taken off the ventilator.
It was something quite amazing to see him awake after a week of seeing him asleep or sedated. I kept him company while the nurse prepared but I was asked to take a walk while they removed his tubes. The nurses said he definitely found his voice again and was doing fine but would need a bit of pressure assistance which was ok. I jumped and cheered in the ward when I saw him free of the ventilator - such a nerd.
His surgeon said the chest infection and his struggle with breathing was a setback but he was doing really well and all it takes now is some patience to allow him to recover at his own pace. It boggles my mind that he went from being on a ventilator, off the ventilator, on the respirator, off the respirator and then back on the ventilator and off again all in one week. But, all that matters is he is out of danger and improving...little by little he is moving forward.
Got milk?

With Michael receiving a limited controlled amount of breastmilk in ICU, I found myself sitting with a whole lot of breastmilk going nowhere except down the drain. This was fun for the first 2 days because I allowed myself a glass of wine and I could finally eat a bit of dark chocolate.
But then the novelty wore off and I wondered what to do with all the milk I had to continue expressing. And that's when I decided to donate my milk. I called Milk Matters and made arrangements with them to become a new donor. They told me I could collect bottles from them and, by the following morning, I was well on the wagon for milk donation. After just 3 days, I've filled almost 15 bottles and my freezer looks like a milk depot LOL!
So why donate?
It occurred to me that the reason I was continuing this crazy routine of pumping every 3-4 hours was to give my baby the best nutrition possible. For many moms and babies, this isn't possible and there are helpless little babies who would benefit greatly from receiving breastmilk. With my own child in ICU, I wanted to be able to do a small bit to help another baby and all it would cost me is the time expressing which I was already doing. Donating was a win-win situation for both me and Milk Matters.
Now my routine is to express for Michael in the morning and then my donated feeds are the afternoon and evening. I am hoping to continue donating for as long as possible because I only discovered Milk Matters shortly after Wren went on to formula feeding and it's something I have been wanting to do since then. While I never know where this milk will go eventually, it does brighten our situation to know that I am doing just a small bit to help other children grow big and strong.
Breathe
Oh how things have changed...
24 hours post op, Michael was performing like a champion. Got off his respirator, was holding his own and everything was hunky dory. By 48 hours post op, he wasn't doing so good anymore. He went back on the respirator for breathing assistance and he was getting weaker.
Yesterday, we were informed he has a chest infection. He's getting vitamin supplements, antibiotics, regular physiotherapy and suction to get as much of the fluid secretions off his lungs as possible. We don't know when he'll be leaving ICU but he's getting all the help they can provide to deal with the infection.
This morning he was rather wheezy despite physio and suction but he wasn't breathing as hard or uncomfortably has yesterday. It's not nice to see him have to work so hard to breathe but the oxygen he's receiving does help quite a bit.
I officially got a bit stressed yesterday when there was little change. Spent most of the past two days at hospital although I don't get to see him for much of that time. I try to not hang around in the ICU ward too much because I know the nurses need to focus and work without a parent hovering. Also, I can't do anything really while I am in there. He's sleeping so I talk to him for a bit and stroke his arm or his tummy. After 10 minutes, it's hard to not feel like you're in the way so I prefer to pop in for short visits more regularly than lurk for too long.
For all of us, the only thing we can do now is just breathe...relax, take things as they come and go from there.
24 hours post op, Michael was performing like a champion. Got off his respirator, was holding his own and everything was hunky dory. By 48 hours post op, he wasn't doing so good anymore. He went back on the respirator for breathing assistance and he was getting weaker.
Yesterday, we were informed he has a chest infection. He's getting vitamin supplements, antibiotics, regular physiotherapy and suction to get as much of the fluid secretions off his lungs as possible. We don't know when he'll be leaving ICU but he's getting all the help they can provide to deal with the infection.
This morning he was rather wheezy despite physio and suction but he wasn't breathing as hard or uncomfortably has yesterday. It's not nice to see him have to work so hard to breathe but the oxygen he's receiving does help quite a bit.
I officially got a bit stressed yesterday when there was little change. Spent most of the past two days at hospital although I don't get to see him for much of that time. I try to not hang around in the ICU ward too much because I know the nurses need to focus and work without a parent hovering. Also, I can't do anything really while I am in there. He's sleeping so I talk to him for a bit and stroke his arm or his tummy. After 10 minutes, it's hard to not feel like you're in the way so I prefer to pop in for short visits more regularly than lurk for too long.
For all of us, the only thing we can do now is just breathe...relax, take things as they come and go from there.
An unexpected joy
Before Michael's surgery, we were told to go pass the time and come back at noon. That's precisely what we did but, due to a crisis with another baby in ICU, we had to go to the waiting area. After a while, I went to get a snack and, when I got back, I found Trevor chatting to the woman who was sitting across from us.
Well, her name is Casey. She and her family are from the USA, her husband works for UNICEF and they live in Uganda. When I left the waiting area, Dr Vosloo came to speak to Trevor and also spoke to her about her daughter. She remarked that our children had similar cases so Trevor and Casey started chatting.
It turns out that her family's story is almost identical to ours. They have a 2 year old daughter, had a great 2nd pregnancy, found out their daughter Sasha has Down Syndrome when she was 10 days old and they learnt of her heart defect shortly after. There are, of course, a few differences. Sasha's defect is somewhat different to Michael's, she's a bit older than him and she had to have a repair done although the original plan was for her to also do the PA banding before repair next year.
Anyhoo, medical stuff aside, we had such a great talk about the experience of receiving the diagnosis, all the emotional difficulties, managing a toddler and all this info with a newborn. We talked about the feelings, peoples' response, plans for the future and research. It was incredible to find another family who experienced everything we had experienced.
Casey's done quite a lot of research and she's a teacher so she's passed on some great information to me and we're giving them tips on doctors and stuff here in SA. Because they live in Uganda, her approach to Sasha and Down Syndrome is very practical and hands-on due to the lack of infrastructure and support they have there. Trevor and I are also quite keen on that because we want to be able to support Michael in any way we can with early intervention.
It's something of a miracle that we met these great people and that we clicked so quickly. I said to Casey today that it's going to be quite nice to have a day or two in the paeds ward together so I can meet her daughter properly and she can see Michael. They'll only be in Cape Town for another 3 weeks so I hope we'll all be able to get together with the kids outside of hospital before they head back home. Seems we got a healthier kiddo and some new friends.
Well, her name is Casey. She and her family are from the USA, her husband works for UNICEF and they live in Uganda. When I left the waiting area, Dr Vosloo came to speak to Trevor and also spoke to her about her daughter. She remarked that our children had similar cases so Trevor and Casey started chatting.
It turns out that her family's story is almost identical to ours. They have a 2 year old daughter, had a great 2nd pregnancy, found out their daughter Sasha has Down Syndrome when she was 10 days old and they learnt of her heart defect shortly after. There are, of course, a few differences. Sasha's defect is somewhat different to Michael's, she's a bit older than him and she had to have a repair done although the original plan was for her to also do the PA banding before repair next year.
Anyhoo, medical stuff aside, we had such a great talk about the experience of receiving the diagnosis, all the emotional difficulties, managing a toddler and all this info with a newborn. We talked about the feelings, peoples' response, plans for the future and research. It was incredible to find another family who experienced everything we had experienced.
Casey's done quite a lot of research and she's a teacher so she's passed on some great information to me and we're giving them tips on doctors and stuff here in SA. Because they live in Uganda, her approach to Sasha and Down Syndrome is very practical and hands-on due to the lack of infrastructure and support they have there. Trevor and I are also quite keen on that because we want to be able to support Michael in any way we can with early intervention.
It's something of a miracle that we met these great people and that we clicked so quickly. I said to Casey today that it's going to be quite nice to have a day or two in the paeds ward together so I can meet her daughter properly and she can see Michael. They'll only be in Cape Town for another 3 weeks so I hope we'll all be able to get together with the kids outside of hospital before they head back home. Seems we got a healthier kiddo and some new friends.
24 Hours Post Op
How's Michael doing? (We know that's the question everybody wants answered)
We are happy to say that he is doing really well.
Firstly, the nurses were impressed with how he held up during surgery and he's been strong in ICU. He was given additional fluids, blood and breathing assistance from a respirator plus he was to be kept under sedation for the first 24-36 hours after surgery. It looks and sounds like a bad situation but it really isn't. When we saw him an hour after surgery, I was surprised at how healthy he looked. Not at all pale or worn from the operation.
It was really weird coming home with no baby. Trevor and I laughed at how we kept thinking he was sleeping in his bed so we had to remind ourselves there was no need to be quiet, keep the lights low or plan everything around an evening feed. So, we indulged a lovely soak in the bath, watched Suits in bed and had 8 undisturbed hours of deep sleep.
I went to the hospital after church to see how the little guy was getting on. His ICU nurse told me he was being rather lazy and didn't want to breathe on his own on her first attempt to remove his respirator. I spoke to him for a few minutes and he was moving and wiggling in his sleep. So, the head nurse and the physio said it was time to try taking him off the respirator again as his breathing pattern had improved in the hour since their first attempt. And, he was indeed ready as he started breathing just fine on his own once the apparatus was removed.
Now that he is minus a few tubes, the next step is to give him some breastmilk since he's only been receiving fluids via a drip since the operation. I feel like a cow being milked on a regular basis. I really do take my hat off to women who pump exclusively because this expressing milk thing for every feed is a bit hectic.
Trevor will be visiting Michael this evening to hear what the plan of action is for tomorrow but the ICU nurse says he is doing great for such a small person. She also says that every time she tries to get him to lie straight, he twists himself off to the left...that's my boy! Still doing whatever he likes even under heavy medication and with tubes in his nose LOL!
We are happy to say that he is doing really well.
 |
| Can still see dem chubby cheeks under the tubes |
It was really weird coming home with no baby. Trevor and I laughed at how we kept thinking he was sleeping in his bed so we had to remind ourselves there was no need to be quiet, keep the lights low or plan everything around an evening feed. So, we indulged a lovely soak in the bath, watched Suits in bed and had 8 undisturbed hours of deep sleep.
I went to the hospital after church to see how the little guy was getting on. His ICU nurse told me he was being rather lazy and didn't want to breathe on his own on her first attempt to remove his respirator. I spoke to him for a few minutes and he was moving and wiggling in his sleep. So, the head nurse and the physio said it was time to try taking him off the respirator again as his breathing pattern had improved in the hour since their first attempt. And, he was indeed ready as he started breathing just fine on his own once the apparatus was removed.
 |
| Looking good 27 hours after surgery |
Now that he is minus a few tubes, the next step is to give him some breastmilk since he's only been receiving fluids via a drip since the operation. I feel like a cow being milked on a regular basis. I really do take my hat off to women who pump exclusively because this expressing milk thing for every feed is a bit hectic.
Trevor will be visiting Michael this evening to hear what the plan of action is for tomorrow but the ICU nurse says he is doing great for such a small person. She also says that every time she tries to get him to lie straight, he twists himself off to the left...that's my boy! Still doing whatever he likes even under heavy medication and with tubes in his nose LOL!
Hello Hospital
 |
| "So they call you Superman..." |
In the past two months, both my children have been in hospital. I told my friends with Michael's stay that I suspected it wouldn't be my last time in a paediatrics ward and I was right as we discovered Michael's heart defect and Wren was admitted less than a week later with massive infections.
Now, we're doing hospital yet again. This time I'm in an unfamiliar hospital and 30kms away from home.
I have to say that Chris Barnard Memorial has been pretty good so far. Admission was quick, the nurses in the paeds ward are very warm, friendly and helpful and they were quite efficient in getting all Michael's tests done.
We blitzed through chest X-rays, an ECG, swabs, weighing him and getting him hooked up to the pulse/Ox machine in under 2 hours. The only unpleasant experience was his blood draw which was not only long but difficult. Let's just say the nurse didn't do the most efficient job and it hurt much more than it should. Daddy Trev wasn't impressed at all and we all felt a bit traumatized after it was done.
Michael got fed, wrapped in a blanket and left to sleep off the busy time he had coming into hospital while Mommy and Daddy went to get a much needed meal.
 |
| Trevor sitting in the afternoon sun passing the time |
Michael's surgery is taking place at 09:30 which means he has to get his last milk feed at 03:00...yup, I have to set my alarm and feed him then for the first time in weeks. He has to get a serious bath before surgery so that's happening at 05:30 and he then he can't get any fluids from 6am, yikes! They'll start prepping him for surgery from 08:00, his operation will begin at 09:30 and then he'll be done somewhere between 11:30 and noon. That's one helluva morning for all of us!
Now that I know how hectic tonight and tomorrow morning are going to be, I'm nervous. Part of me wants to sleep and another part of me is too nervous to close my eyes and start the cycle of broken sleep for the night. I'm also nervous because Michael will be denied milk while he's awake and being prepped for surgery and that's pretty hectic for an 8 week old who spends his days doing nothing but feeding and sleeping. He has yet to take a bottle which compounds the situation but I guess we're just going to have to make do and improvise.
It's been wonderful receiving so many heartfelt messages offering prayers and thoughts for the little guy. It means the world to us and we know so many people are carrying us in their hearts. I want to get a plane to sky write "thank you" because that's the biggest font size possible and even that doesn't fully cover the true enormity of the gratitude we feel. There's that thing on the back of taxis which reads "When days are dark, friends are few" Well, not for us. Our days are quite bright and it's thanks to the many people; friends, family, doctors and nurses, who are helping us and guiding us through this experience.
Thanks to you all from the bottom of our hearts xoxo
A broken heart
As Michael entered his 4th week, he developed major nasal congestion. It got so bad that he started setting off his Angelcare monitor while he struggled to breathe past all the gunk in the back of his nose.
I took him straight to his paediatrician who confirmed he definitely had bad congestion but he was concerned about the monitor going off. He admitted Michael to hospital for apnea observation and we agreed to him running a battery of tests on Michael which would have to be done anyway at some or other time.
So, off we went to Mediclinic Durbanville for a 48 hour stay. There were blood tests, X-rays, ultrasound, an ECG and an appointment with a paediatric cardiologist for a thorough look at his heart. All the tests were fine albeit tiring and Michael was quite the trooper with all the positioning, poking and prodding going on.
The big one was the cardiologist's appointment. The little guy slept through his cardiac ultrasound and it was a good thing because it gave us time to process the news we received.
Michael has an atrioventricular septal defect. Children with Trisomy 21 often have a heart condition and he has one of the more common varieties. I've included a picture which illustrates the defect here.
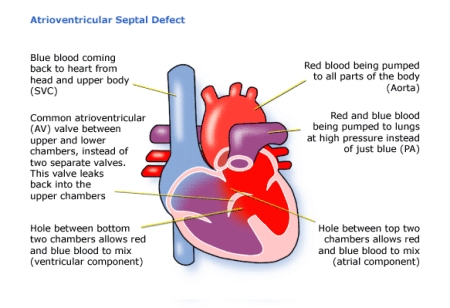
In Michael's case, the defect is quite complicated so a full repair won't happen until he's a toddler. To help his body cope, he is getting a pulmonary artery banding. This will reduce the excess blood flowing through his lungs to only what he needs and take some strain off his heart until the repair can happen. He still has good blood flow and little mixing but the defect is creating flow imbalances to his other organs and his heart is enlarged.
When we heard this, we weren't even shocked. We were kind of expecting things to go wrong and to hear more bad news. However, this is something that can be fixed and he has the best paediatric heart surgeon in the country. It's not great knowing our infant is undergoing major surgery but it's better than him suffering through heart failure which is the eventual complication of his defect.
The surgery is taking place on 25 July at Christiaan Barnard Memorial hospital and it's going to be a 7-10 day stay while he recovers. The surgeon, Dr Susan Vosloo, is very confident there will be no problems and he is healthy in every other way so he's in good condition for surgery.
We aren't nervous (yet) for the surgery, more concerned about Michael after. It's not nice to see a little baby who cannot communicate that he is pain and we wonder how he'll be fed when the incision is on his side. Dr Vosloo assured us that he will be pain free or comfortable at the least as they like to make sure the babies are cared for. As for feeding, well we'll have to see how to cross that bridge when we get there.
It's going to be weird leaving Michael in ICU while I come home but I am learning to let go and trust in others tasked with caring for this little person. I have come around to the conclusion that what must be will be and all I can do is have faith.
I took him straight to his paediatrician who confirmed he definitely had bad congestion but he was concerned about the monitor going off. He admitted Michael to hospital for apnea observation and we agreed to him running a battery of tests on Michael which would have to be done anyway at some or other time.
So, off we went to Mediclinic Durbanville for a 48 hour stay. There were blood tests, X-rays, ultrasound, an ECG and an appointment with a paediatric cardiologist for a thorough look at his heart. All the tests were fine albeit tiring and Michael was quite the trooper with all the positioning, poking and prodding going on.
The big one was the cardiologist's appointment. The little guy slept through his cardiac ultrasound and it was a good thing because it gave us time to process the news we received.
Michael has an atrioventricular septal defect. Children with Trisomy 21 often have a heart condition and he has one of the more common varieties. I've included a picture which illustrates the defect here.
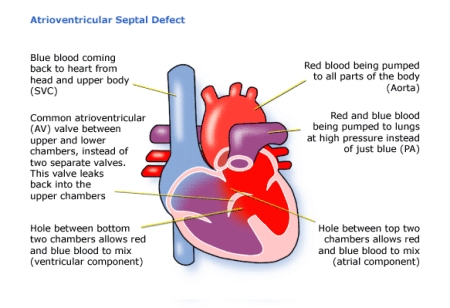
In Michael's case, the defect is quite complicated so a full repair won't happen until he's a toddler. To help his body cope, he is getting a pulmonary artery banding. This will reduce the excess blood flowing through his lungs to only what he needs and take some strain off his heart until the repair can happen. He still has good blood flow and little mixing but the defect is creating flow imbalances to his other organs and his heart is enlarged.
When we heard this, we weren't even shocked. We were kind of expecting things to go wrong and to hear more bad news. However, this is something that can be fixed and he has the best paediatric heart surgeon in the country. It's not great knowing our infant is undergoing major surgery but it's better than him suffering through heart failure which is the eventual complication of his defect.
The surgery is taking place on 25 July at Christiaan Barnard Memorial hospital and it's going to be a 7-10 day stay while he recovers. The surgeon, Dr Susan Vosloo, is very confident there will be no problems and he is healthy in every other way so he's in good condition for surgery.
We aren't nervous (yet) for the surgery, more concerned about Michael after. It's not nice to see a little baby who cannot communicate that he is pain and we wonder how he'll be fed when the incision is on his side. Dr Vosloo assured us that he will be pain free or comfortable at the least as they like to make sure the babies are cared for. As for feeding, well we'll have to see how to cross that bridge when we get there.
It's going to be weird leaving Michael in ICU while I come home but I am learning to let go and trust in others tasked with caring for this little person. I have come around to the conclusion that what must be will be and all I can do is have faith.
Supermassive Black Hole
Normally, I'm able to associate music to situations in my life. The week after Michael's Down Syndrome diagnosis has no music because there is no sound, no lyric, no rhythm that can describe the darkness that came over me.
I like to describe myself as a scientist with a little creative sprinkled on top. Because I function with facts, I spent the first few days after the diagnosis reading...and reading far too much. I scheduled an appointment with a genetic counsellor so we could get a better understanding of what this condition means for parents. There was just so much information and my brain was spinning at 4000 km/s.
I spent my days weeping in the shower, tearing up with every feed and just feeling lost, angry, sad and confused. How the heck did we end up with this?!?!
The genetic counsellor was great and answered all of our questions. We had all this information and set off to Arabella for a weekend of rest. Or so I thought.
As Friday night drifted into the early hours of Saturday morning, I hit my breaking point. I was feeding Michael in the dark and thinking a few things at the same time: Why did God do this to us? What kind of god places such a burden on an innocent child doomed to spend life being different and incapable of independence? Wouldn't it just be better if he hadn't been born in the first place? How lonely is he going to feel when he learns he will never marry or have children? How are we going to cope with a special needs child? What happens to all our dreams for the future?
There were just a lot of thoughts and, at my lowest point, I detached emotionally from Michael. I looked at him and felt nothing. When I wasn't looking at him, I felt pain and a deep, deep sense of loss. I was in mourning because I felt I had been robbed of the son I had prayed for. Honestly, why did God give me what I wanted and, via an extra chromosome, not only take it away from me but also give me a whole new set of problems?
If you had seen me that night, you would've agreed that I really needed some psychological assistance at that point. The next morning, Trevor had the arduous task of bringing me back to life. He spent an hour sitting and talking with me trying to pull me out of a completely negative headspace. Eventually, he got it right and I slowly started returning to normal with a slightly more positive outlook.
I have to say that I'm only explaining my feelings. Trevor also went through a very difficult time for weeks after but I can't speak of what he felt. All I can put down here is my experience. It was awful. They say that receiving that diagnosis is exactly the same as losing someone you love and you do go through the stages of grief. I personally was mourning the loss of the future I hoped for, not only for myself and my family but also for Michael.
It took quite a while for me to make peace with that extra chromosome and what it means. The journey there had plenty of hiccups and, of course, I am still a bit heartbroken that Michael's path ahead isn't easy. I had many days where it felt like I was in a dream waiting to wake up or that I was standing inside someone else's life. But it is what it is and all we can do now is choose how we deal with it. Our friends and family have been incredible pillars of support and they're a big part of how we've been coping. I know Michael is loved and our job now is to help him reach his full potential...whatever that may be.
I like to describe myself as a scientist with a little creative sprinkled on top. Because I function with facts, I spent the first few days after the diagnosis reading...and reading far too much. I scheduled an appointment with a genetic counsellor so we could get a better understanding of what this condition means for parents. There was just so much information and my brain was spinning at 4000 km/s.
I spent my days weeping in the shower, tearing up with every feed and just feeling lost, angry, sad and confused. How the heck did we end up with this?!?!
The genetic counsellor was great and answered all of our questions. We had all this information and set off to Arabella for a weekend of rest. Or so I thought.
As Friday night drifted into the early hours of Saturday morning, I hit my breaking point. I was feeding Michael in the dark and thinking a few things at the same time: Why did God do this to us? What kind of god places such a burden on an innocent child doomed to spend life being different and incapable of independence? Wouldn't it just be better if he hadn't been born in the first place? How lonely is he going to feel when he learns he will never marry or have children? How are we going to cope with a special needs child? What happens to all our dreams for the future?
There were just a lot of thoughts and, at my lowest point, I detached emotionally from Michael. I looked at him and felt nothing. When I wasn't looking at him, I felt pain and a deep, deep sense of loss. I was in mourning because I felt I had been robbed of the son I had prayed for. Honestly, why did God give me what I wanted and, via an extra chromosome, not only take it away from me but also give me a whole new set of problems?
If you had seen me that night, you would've agreed that I really needed some psychological assistance at that point. The next morning, Trevor had the arduous task of bringing me back to life. He spent an hour sitting and talking with me trying to pull me out of a completely negative headspace. Eventually, he got it right and I slowly started returning to normal with a slightly more positive outlook.
I have to say that I'm only explaining my feelings. Trevor also went through a very difficult time for weeks after but I can't speak of what he felt. All I can put down here is my experience. It was awful. They say that receiving that diagnosis is exactly the same as losing someone you love and you do go through the stages of grief. I personally was mourning the loss of the future I hoped for, not only for myself and my family but also for Michael.
It took quite a while for me to make peace with that extra chromosome and what it means. The journey there had plenty of hiccups and, of course, I am still a bit heartbroken that Michael's path ahead isn't easy. I had many days where it felt like I was in a dream waiting to wake up or that I was standing inside someone else's life. But it is what it is and all we can do now is choose how we deal with it. Our friends and family have been incredible pillars of support and they're a big part of how we've been coping. I know Michael is loved and our job now is to help him reach his full potential...whatever that may be.
The day our life changed
At my 16 week check-up, my gynae started the appointment by expressing her displeasure with me. I was supposed to go for a blood test at 12 weeks which I forgot about and only had it done a week before my next appointment. The test indicated an increased risk of Down Syndrome.
Trevor and I were sent off to a specialist who couldn't make a conclusive diagnosis and we declined amniocentesis. The specialist felt that if we weren't going to terminate, there was no point in doing the amnio and risking a healthy child who showed no other indications of Trisomy 21 except for that one blood test.
For the rest of my pregnancy, my doctor checked for every marker and none showed up. I even had a 3D ultrasound on a shoot for work and that gynae who didn't know me remarked that the baby showed no signs of Trisomy 21. And so we all hoped and prayed everything was fine.
The day after Michael's birth, the paediatrician examined him thoroughly again and said he had some concerns. Michael didn't show enough of the physical characteristics for him to make a diagnosis and we all felt a blood test would answer everybody's question. For the next week, we were just a normal family with two children adjusting to life with a newborn.
And then the paediatrician asked to see us. He examined Michael yet again and, after that, we sat down and he delivered the news: Michael's blood test confirmed he has Trisomy 21.
I held my composure while he explained the situation to us and we listened to the information he provided. But, when we got into the car, the walls came down and so did the tears. I cried bitterly all through Michael's feed and most of that afternoon is a blur.
In just a few seconds, Michael's entire future was ripped from us. The boy I imagined playing soccer at school, giving me grief during high school, partying during his university days, getting married and having kids was gone. Those images were burnt in my mind and we were left with nothing but black.
Despite knowing there was a risk, nothing prepared us for the reality. And to make matters worse, Trevor had to rush off with Wren-Lee to the doctor as she was sick and steadily deteriorating. We were tired emotionally and physically and had to prepare ourselves for what was coming...
Michael's birth story
At my very first antenatal appointment, my gynae said, "I wonder what this one's birth story is going to be."
What she meant by that was whether or not this child would have an interesting story like Wren's. Well, he does have a story...and it is something crazy and incredible.
At 35 weeks, I got the flu. I tried to go to work on two separate days but I was exhausted and not holding up well. On top of that, Michael was kicking and wriggling much more than usual and it only added to my discomfort. I saw my gynae on the Friday as she was leaving the next day on a three week holiday in Europe and would be returning right before the date we planned for a C-section if necessary. She was concerned about my health and that of the baby so, she booked me off work for an extra week to recover. We had a look at Michael, he was fine and the last thing she said was that this baby just needed to wait for her to come back.
Resting is something I don't do well and being forced to do very little for a week was more agony than enjoyable. By the Monday, I felt much better although still heavily congested. I was up and about doing stuff and felt good about the day. When I woke up the next day, it was completely different. I was freezing cold, just couldn't warm up and I was unbelievably tired.
Trevor, Wren-Lee and I all went to bed early because he was set to fly to Durban at 06:30 the next morning. We lay in bed chatting briefly and I was still awake for about 20 mins after Trevor had fallen asleep. While I lay there thinking, I felt a pop and warm liquid running down my leg. I knew immediately that my water just broke.
I woke Trevor up (and Wren-Lee jumped up too), called my parents and then tried to figure out how to get out of my bed without soaking the floor. It was pretty comical and I laughed while Trevor explained to Wren what was happening. With her safely off with my parents, I realised we had a slight problem seeing as I hadn't packed for hospital and didn't have everything I needed. But, there was no time to stress about it so we went off to hospital with whatever I could gather at 11pm.
The nurses called Dr Truter who was looking after all my gynae's patients in her absence. He advised a sleeping tablet and rest. Trevor went home and I went to sleep...until 4am. The contractions become more prominent and it started to hurt. By 8am, Dr Truter came to introduce himself and have a talk. Because I was 36 weeks along, there was no plan. He examined me, felt another c-section was the best course of action and it was set for lunchtime. I was really sore and he gave the go ahead for me to get a shot of Pethidine. I got the next shot an hour later and still the pain got worse. Another hour later, I got my third shot of Pethidine and strapped into the monitor.
My contractions were incredibly painful and I started asking if I could get an epidural for a few hours till my delivery. Request denied: It wouldn't be necessary if the baby was being born so soon. Trevor had the unpleasant job of rubbing my back with every contraction as I tried to breathe my way through them which was tough with heavy nasal congestion. By 11:50, I demanded to be freed from the monitor around my belly and ran for the shower. The hot water on my back finally brought relief and I refused to leave as my contractions were on top of one another. Trevor was begging me to get into my surgical gown so I could be wheeled to theater and I refused to leave the bathroom. Ironically, my stubbornness in that moment is what changed the game.
I eventually got into the gown, back in the bed and was wheeled into the passage en route to theater. Just as we were about to leave the maternity ward, I felt something change, a strong urge to push and I screamed. The nurse looked under my blanket and realised that this baby was coming out now. They turned me around and rushed me into a delivery room.
By now I was exhausted, begging for oxygen and saying I couldn't deliver this baby. I was seeing stars from lack of oxygen and in extreme pain. Between the midwife, the gynae and Trevor, I was getting three streams of information and instruction and there was no time for any painkillers so I was going au naturel. Lots of screaming, shouting and six pushes later, there was a baby.
The first question I asked as I watched Trevor and the paediatrician inspect the new little person with the big voice was for the time. It wasn't even 1pm yet. Apparently it was just 10 minutes from the time I was wheeled into delivery until Michael was born. This kid fought his way out into the world on his own terms.
I had wanted a natural delivery from the time I found out about the pregnancy, and although it definitely didn't go the way I planned, it was an amazing experience. The next day the gynae explained that I dilated the last 4 cms in less than an hour before I delivered so my contractions were incredibly painful and my exhaustion and rather loud reactions were valid. Michael's birth was definitely unexpected but he surprised us all with quite a story.
What she meant by that was whether or not this child would have an interesting story like Wren's. Well, he does have a story...and it is something crazy and incredible.
At 35 weeks, I got the flu. I tried to go to work on two separate days but I was exhausted and not holding up well. On top of that, Michael was kicking and wriggling much more than usual and it only added to my discomfort. I saw my gynae on the Friday as she was leaving the next day on a three week holiday in Europe and would be returning right before the date we planned for a C-section if necessary. She was concerned about my health and that of the baby so, she booked me off work for an extra week to recover. We had a look at Michael, he was fine and the last thing she said was that this baby just needed to wait for her to come back.
Resting is something I don't do well and being forced to do very little for a week was more agony than enjoyable. By the Monday, I felt much better although still heavily congested. I was up and about doing stuff and felt good about the day. When I woke up the next day, it was completely different. I was freezing cold, just couldn't warm up and I was unbelievably tired.
Trevor, Wren-Lee and I all went to bed early because he was set to fly to Durban at 06:30 the next morning. We lay in bed chatting briefly and I was still awake for about 20 mins after Trevor had fallen asleep. While I lay there thinking, I felt a pop and warm liquid running down my leg. I knew immediately that my water just broke.
I woke Trevor up (and Wren-Lee jumped up too), called my parents and then tried to figure out how to get out of my bed without soaking the floor. It was pretty comical and I laughed while Trevor explained to Wren what was happening. With her safely off with my parents, I realised we had a slight problem seeing as I hadn't packed for hospital and didn't have everything I needed. But, there was no time to stress about it so we went off to hospital with whatever I could gather at 11pm.
The nurses called Dr Truter who was looking after all my gynae's patients in her absence. He advised a sleeping tablet and rest. Trevor went home and I went to sleep...until 4am. The contractions become more prominent and it started to hurt. By 8am, Dr Truter came to introduce himself and have a talk. Because I was 36 weeks along, there was no plan. He examined me, felt another c-section was the best course of action and it was set for lunchtime. I was really sore and he gave the go ahead for me to get a shot of Pethidine. I got the next shot an hour later and still the pain got worse. Another hour later, I got my third shot of Pethidine and strapped into the monitor.
My contractions were incredibly painful and I started asking if I could get an epidural for a few hours till my delivery. Request denied: It wouldn't be necessary if the baby was being born so soon. Trevor had the unpleasant job of rubbing my back with every contraction as I tried to breathe my way through them which was tough with heavy nasal congestion. By 11:50, I demanded to be freed from the monitor around my belly and ran for the shower. The hot water on my back finally brought relief and I refused to leave as my contractions were on top of one another. Trevor was begging me to get into my surgical gown so I could be wheeled to theater and I refused to leave the bathroom. Ironically, my stubbornness in that moment is what changed the game.
I eventually got into the gown, back in the bed and was wheeled into the passage en route to theater. Just as we were about to leave the maternity ward, I felt something change, a strong urge to push and I screamed. The nurse looked under my blanket and realised that this baby was coming out now. They turned me around and rushed me into a delivery room.
By now I was exhausted, begging for oxygen and saying I couldn't deliver this baby. I was seeing stars from lack of oxygen and in extreme pain. Between the midwife, the gynae and Trevor, I was getting three streams of information and instruction and there was no time for any painkillers so I was going au naturel. Lots of screaming, shouting and six pushes later, there was a baby.
The first question I asked as I watched Trevor and the paediatrician inspect the new little person with the big voice was for the time. It wasn't even 1pm yet. Apparently it was just 10 minutes from the time I was wheeled into delivery until Michael was born. This kid fought his way out into the world on his own terms.
I had wanted a natural delivery from the time I found out about the pregnancy, and although it definitely didn't go the way I planned, it was an amazing experience. The next day the gynae explained that I dilated the last 4 cms in less than an hour before I delivered so my contractions were incredibly painful and my exhaustion and rather loud reactions were valid. Michael's birth was definitely unexpected but he surprised us all with quite a story.
Subscribe to:
Comments (Atom)
